Data Requirements for Step 2: Preclinical Studies
7.1 Prerequisites for Conducting Preclinical Studies
Preclinical studies Before initiating preclinical studies, the applicant must adhere to RCGM guidelines, which include demonstrating the consistency of the process and product, characterizing the product, and establishing product specifications. The applicant is required to submit generated data alongside essential clinical information and preclinical study protocols to the RCGM for approval. Toxicology studies should commence only after receiving RCGM authorization.
Basic Information on Reference Biologics Preclinical Studies
- Drug Information: Includes details on the drug, administration route, absorption and elimination rates, therapeutic index, dosing, vehicle, administration mode, and dose-response relationships.
- Bioequivalence: Provide available data on bioequivalence ranges.
- Localization: Information on tissue-specific localization, if available.
- Toxicity Data: Available toxicity information regarding the Reference Biologic.
- Mechanism of Action: Details on how the drug works.
Basic Information on Similar Biologics
- Clinical Use: Known or proposed clinical applications.
- Target Population: Information on age, sex, pregnancy status, lactation, and pediatric considerations.
- Dosage Information: Frequency, intervals, and units of administration.
- Administration Routes: Primary and alternate routes for drug delivery.
- Final Formulation: Composition details, including adjuvants and additives, along with toxicology data for these components.
- Diluents: Information on any diluents used.
- Presentation: Format of the product, such as pre-filled syringes, cartridges, or vials.
Application Requirements for RCGM
The application submitted to RCGM must include the approval from the Institutional BioSafety Committee (IBSC) of the developer, along with a copy of the meeting minutes. Additionally, if available, approval from the Institutional Animal Ethics Committee (IAEC) should be provided. The applicant must also detail the proposed site for toxicity testing, including information on the personnel involved, such as the study director, principal investigator, pathologist, other investigators, and the quality assurance officer. It is also necessary to provide the status of GLP certification for the proposed facility. FDA requirement
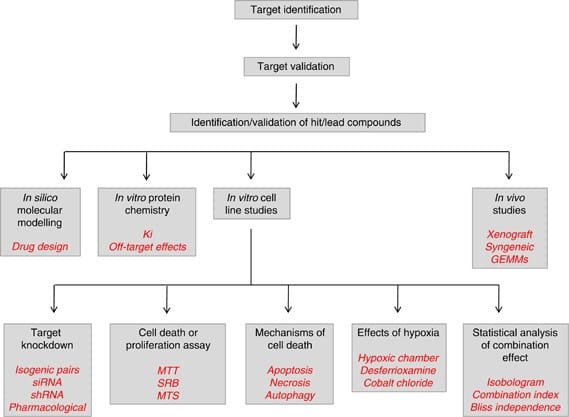
7.2 Preclinical Studies (Pharmacodynamics and Toxicology)
Preclinical studies must be completed before any clinical trials commence. These studies should be comparative, aimed at identifying any differences between the Similar Biologic and the Reference Biologic. The design of these studies may vary based on clinical parameters such as therapeutic index and the types of indications being pursued.
The rationale for the chosen approach must be thoroughly justified in the preclinical overview. Studies should utilize the final formulation of the Similar Biologic intended for clinical use, as well as that of the Reference Biologic, unless a justification is provided otherwise. The dosage form, dose, strength, and administration route of the Similar Biologic must align with those of the Reference Biologic; any discrepancies must be justified. The following studies are required for preclinical evaluation:
7.2.1 Pharmacodynamic Studies
- In Vitro Studies: The comparability between the Similar Biologic and the Reference Biologic must be demonstrated through in vitro cell-based bioassays. These may include assays for cell proliferation, cytotoxicity, neutralization, and receptor binding.
- In Vivo Studies: In vivo assessments of biological or pharmacodynamic activity may not be necessary if reliable in vitro assays are available that accurately reflect the pharmacodynamic activity of the Reference Biologic. However, if the in vitro assays do not adequately represent the pharmacodynamics, then in vivo studies should be conducted as needed.
7.2.2 Toxicological Studies
For in vivo toxicity assessments, it is essential to conduct at least one repeat-dose toxicity study using a pharmacologically relevant species with the intended administration route. The applicant must provide scientific rationale for the selection of animal models based on existing literature. If the appropriate pharmacologically relevant species is unavailable and properly justified, studies may proceed using rodent or non-rodent species as stipulated by Schedule Y, pending approval from RCGM.
The administration route must align with the intended route specified in Schedule Y, whether using pharmacologically relevant or non-relevant animal models. Typically, the duration of these studies should be a minimum of 28 days, including a recovery period of 14 days, although this may vary based on dosage and other specific factors.


Doses should be determined based on the therapeutic dose of the Reference Biologic. If necessary, a pilot dose-response study should be conducted prior to the main toxicity studies. Generally, three dosage levels—low, medium, and high—corresponding to 1X, 2X, and 5X of the human equivalent dose (HED) or higher, will be used in repeated-dose toxicity studies. In these studies, the Similar Biologic must be compared to the Reference Biologic at least at the 1X HED level. Any differences in dosage levels must be justified and approved before the studies commence. The administration schedule can be based on therapeutic protocols.
Depending on the route of administration, an evaluation of local tolerance should be conducted. If feasible, this assessment may be integrated into the aforementioned repeated-dose toxicity study.
Study Groups for Repeated-Dose Toxicity Testing
The study groups in repeated-dose toxicity testing will include:
- Historical Control (optional)
ii. Vehicle Control
iii. Vehicle Control for the recovery group
iv. Formulation without protein (for vaccines), with each adjuvant assessed independently
v. 1X Similar Biologic (lowest dose) for the study duration
vi. 1X Reference Biologic for the study duration
vii. 2X Medium dose Similar Biologic
viii. 5X High dose Similar Biologic
ix. Similar Biologic with a recovery group extending 7 to 14 days beyond the study period
Protocols and Study Reports
The study protocols and reports must include comprehensive details on the following aspects of toxicity testing:
- Pre-euthanasia Procedures: Document actions such as blood collection and body weight measurements.
- Post-euthanasia Events: Include necropsy details, gross descriptions, organ weights, and a list of organs sampled for histopathology.
- Biochemical Parameters: Outline the equipment and methods used, including units of measurement.
- Hematology Procedures: Specify the methods (automated or manual) and parameters evaluated.
- Statistical Methods: Describe the statistical techniques employed in data analysis.
- Bone Marrow Examination: Indicate whether bone marrow was assessed through aspirate, smear, or histopathology sections.
Histopathological Observations
For histopathological evaluations, applicants should consider the following:
- Document any deviations from standard histology, noting the incidence in different groups.
- Determine the significance of observed features based on statistical analysis, dose-response relationships, or their alignment with normal ranges in biochemical and hematological data.
- If not all organs from every animal are examined (e.g., 4 out of 5 livers), provide justification for any exclusions.
- Include proposed actions in the protocol for instances of premature death or morbidity among subjects.
Other Toxicity Studies
Additional toxicity studies, such as safety pharmacology, reproductive toxicity, mutagenicity, and carcinogenicity assessments, are generally not required for evaluating a Similar Biologic unless indicated by the results from the repeated-dose toxicity studies.
Final Study Report Requirements
The final report must encompass all aspects outlined in the approved protocol and include the following sections/documents:
- RCGM approval for the protocol and test center
- IBSC approval of the report
- IAEC approval for animal use and procedures
- Quality assurance statement
- Signatures of the study director and all investigators involved
- Quality analytical reports for the test material and vehicle
- Certifications for animal feed and animal health
- Documentation of any protocol deviations
- A discussion of the results
- Individual animal data, summary data, and any additional outputs, such as computer analysis results
- Conclusions
Immune Responses in Animals
The antibody response to the Similar Biologic should be compared with that generated by the Reference Biologic in an appropriate animal model. Test serum samples must be evaluated for reactions to host cell proteins.
To assess the immune toxicity of the Similar Biologic, the results of local tolerance (from either the repeat-dose study or a standalone test) should be analyzed in conjunction with immunogenicity observations from the sub-chronic study. Thus, immunogenicity testing should be incorporated into the protocols for sub-chronic repeated-dose studies.
Other factors to consider when evaluating immune toxicity include the presence of immune complexes in targeted tissues, which should be examined alongside histopathological observations. Upon completion of the preclinical studies, the reports will be submitted to the RCGM for review and consideration.
Other Toxicity Studies
Additional toxicity studies, such as safety pharmacology, reproductive toxicity, mutagenicity, and carcinogenicity assessments, are typically not required for the evaluation of a Similar Biologic unless the findings from the repeated-dose toxicity studies suggest otherwise.
Upon successful review of the preclinical study reports—which should demonstrate process and product consistency, product characterization, specifications, and comparisons of Similar Biologics to the Reference Biologic—the RCGM will recommend to the DCG(I) that the sponsor be permitted to proceed with the appropriate phase of clinical trials as per CDSCO guidelines. The applicant may submit simultaneous applications to both the RCGM and the DCG(I) office for clinical trial approval. However, the DCG(I) office will finalize its review and grant permission only after receiving the RCGM’s recommendation.